Back when the office looked like Mad Men, appetite suppression wasn’t exactly a medical innovation. It was three scotches before dinner and a pack of cigarettes at the conference table.
Nicotine blunts hunger. Alcohol numbs it.
That was one way to power through a long workday.
Thankfully, we’ve evolved.
Today’s appetite conversation revolves around GLP-1 medications, metabolic health, and pharmacological precision — not ashtrays and highballs.
But the core issue hasn’t changed: high performers still struggle with energy, hunger, and body regulation in demanding environments.
The GLP‑1 era changed the conversation about hunger.
Not because people suddenly became more disciplined—but because we finally admitted the obvious: appetite is biological.
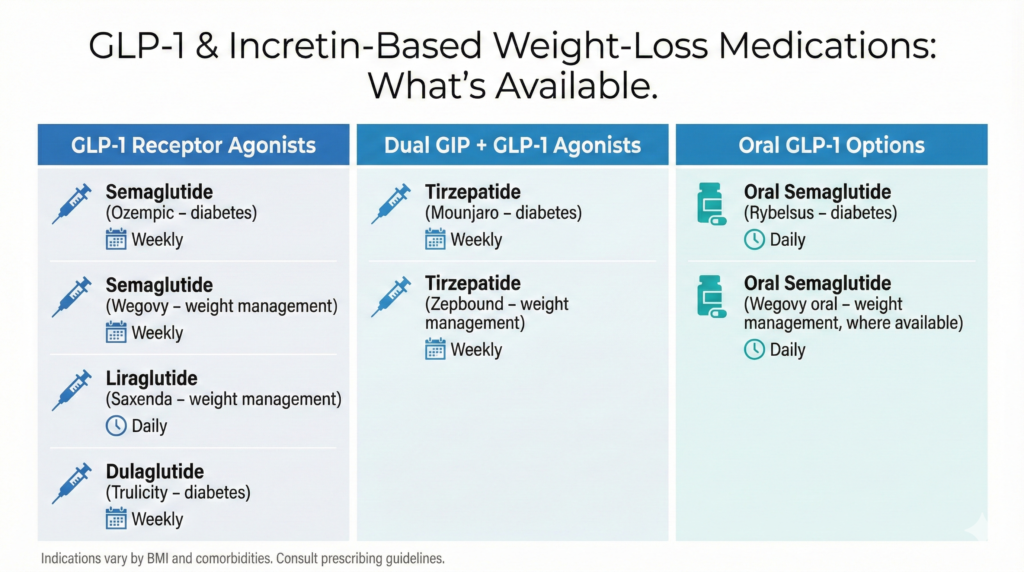
Drugs like Ozempic and its companion medications work largely by reducing energy intake through the brain’s satiety pathways, and by slowing gastric emptying so fullness lasts longer.
For many people, that’s life-changing. For some, it’s medically necessary.
But a lot of us live in the in-between.
Our BMI isn’t high enough to qualify under typical chronic weight-management indications (BMI ≥30, or ≥27 with a weight-related condition). We’re not trying to drop 50 pounds. We’re trying to stay ahead of the quiet creep—three pounds up, five pounds down, repeat—because adult life is stress, computer time, travel, and hormones.
And on top of that, the side-effect discourse is real. Beyond routine GI effects that are well recognized on labels (nausea, constipation, abdominal symptoms), the fact that federal litigation exists around alleged injuries is part of why some professionals don’t want to start this path casually.
So instead of losing the battle, I built a system.
Not a “diet.”
An appetite architecture.
For a Deeper Dive on How GLP-1s Actually Work
If you want a more technical breakdown of how GLP-1 receptor agonists influence appetite, insulin signaling, gastric emptying, and brain satiety centers, I wrote a separate background explainer that walks through the science in plain English.
That piece covers what these medications do mechanistically — including why people feel full faster, why cravings shift, and what typically happens when the drugs are discontinued.
You can read that full analysis here:
Understanding the biology matters — especially if you’re trying to decide whether to use these medications or replicate some of their appetite effects naturally.
My core belief
Weight management after your mid‑30s is not a one-time project. It’s an operating system.
Your body will fluctuate, often for reasons unrelated to fat gain—water, digestion, training inflammation, hormonal shifts. The point isn’t to panic.
The point is to stay proactive enough that the fluctuation never becomes a landslide.
Tactic one: I use a “natural GLP‑1” tool the way an adult uses tools
I started taking a GLP‑1-support powder—specifically HUM Nutrition’s Flatter Me Fiber GLP‑1 Booster—because it’s not pretending to be a drug. It’s basically a satiety-forward fiber tool.
Here’s what’s real about it:
A specific prebiotic fiber (Fibersol‑2 / resistant maltodextrin) has human data showing that taking 10 grams with a meal can increase satiety hormones like GLP‑1 and PYY and reduce hunger in some controlled settings.
And mechanistically, fiber can support GLP‑1 signaling through gut fermentation and SCFAs—again, physiology, not magic.
So I don’t treat this like a miracle. I treat it like a lever.
Tactic two: I protect eight hours of sleep because sleep loss creates “munchie brain”
If you want to feel less hungry, stop treating sleep like optional life admin.
Randomized trials and systematic review evidence show that sleep restriction tends to increase energy intake and appetite/hunger signals. Controlled experiments also link sleep restriction with higher ghrelin and higher calorie consumption when food is available.
In other words: if I’m sleep-deprived, my appetite is not a reliable narrator.
So “eight hours” is not wellness fluff. It’s appetite control.
Tactic three: I use green tea extract as an accelerator—not a daily identity
When I need to tighten up on a more accelerated basis, I sometimes use green tea extract.
The evidence suggests green tea extract can produce modest improvements in weight and body composition on average across randomized trials. But it’s not a guaranteed appetite suppressant, and some analyses show no meaningful effect on leptin/ghrelin.
Also: adults use adult disclaimers.
Green tea extract has a documented (rare) liver injury risk in certain cases and is not something you stack recklessly with other “fat burner” supplements.
Tactic four: I eat “baseline” during the day and save my real meal for dinner
I don’t do big sit-down meals in the middle of my workday.
Partly because a large meal can trigger post-meal drowsiness that feels like a productivity penalty.
So my daytime strategy is simple: satisfy baseline hunger, stay functional, and protect dinner as my main meal.
This is not me recommending extreme restriction for everyone. People respond differently to meal timing, and some studies show that very low meal frequency can increase hunger.
But for me, it’s an execution strategy: I’d rather be sharp all day and eat like a human at night.
Tactic five: I use small “oral fixation” tools instead of snacking
I chew gum.
I drink sparkling water—often something like Pellegrino—because it gives me the sensation of “having something” without turning into a snack spiral.
The gum piece is supported by mixed but legitimate research: systematic review evidence suggests chewing gum can reduce hunger or desire to eat in some contexts, even if weight-loss outcomes are not consistent across studies.
On carbonation: I’m not claiming it suppresses appetite. The evidence is limited, and some small studies raise the possibility carbonation could influence ghrelin. For me, it’s about replacing snacking behavior—not hacking hormones.
Tactic six: I stay active, and I stay on my feet—especially because I work remote
Remote work can quietly increase sedentary time and reduce steps, which changes your baseline energy balance without you noticing.
So I overcorrect: I build movement into the day on purpose.
Not as a fitness identity. As a metabolism and appetite strategy.
Tactic seven: I get dressed immediately—real clothes, real feedback
This might be the most underrated tactic.
Stretchy clothes are forgiving. Too forgiving.
So I get dressed in structured clothing early, including on weekends, because it’s a built-in body check. It’s not about shame—it’s about awareness.
Self-monitoring behaviors are consistently associated with better weight management outcomes, and my wardrobe is one more feedback loop that keeps me honest.
Tactic eight: I go to the gym late afternoon because early workouts make me hungry early
I train daily, and I prefer late afternoon.
Because when I work out in the morning, it makes me hungry earlier—and that’s not compatible with how I run my workday.
Research on exercise timing and appetite is complex. In one controlled trial, morning and evening exercise produced similar subjective appetite responses, but energy intake after exercise was higher following evening sessions—showing that appetite signals and intake don’t always match perfectly.
In DAOFitLife terms: this is why you have to design around your personal pattern, not someone else’s.
The bottom line
This isn’t an anti‑GLP‑1 argument.
This is a pro‑systems argument.
If your weight fluctuates in that annoying adult way, you can either:
- drift and react, or
- build a repeatable appetite system that keeps you ahead of it.
Mine is fiber support, sleep protection, occasional acceleration, intentional meal timing, movement, and constant self-awareness.
Smarter Tech. Stronger Humans.
Professional note
This article is educational and reflects personal routines, not medical advice. If you have diabetes, a history of eating disorders, liver disease, are pregnant, or take prescription medications, talk with a clinician before changing meal timing or adding supplements—especially concentrated green tea extract.






